Article
Catherine S. Chang, MD1 and Scott P. Bartlett, MD2
Abstract
The incidence of congenital ear deformities has been documented to be as high as 58% of all newborns. Unfortunately, the majority of these deformations do not spontaneously self-correct, leaving the child with a permanent deformity that can only be corrected through surgery. With the evolving simplicity of ear molding that can be done in the office, this can obviate the need for unnecessary surgery that comes with its own set of complications and a higher cost. Early detection and early treatment is key for successful ear molding. The purpose of this article is to review the types of deformational ear deformities and the most up-to-date literature on ear molding, increase awareness to this topic, and ultimately increase patient and parental satisfaction with their overall care.
Keywords
ear deformity, ear molding, ear malformation, nonsurgical, congenital ear deformity
Introduction
It has long been taught in medical school and pediatric residency training that deformations of the ear will self- correct and that any intervention in the neonatal period is unnecessary. Recent evidence to the contrary, that a significant majority of these do not self-correct, demands that pediatricians and neonatologists be able to not only recognize the pattern and types of deformation but assume a pivotal role in the early management of these differences. The purpose of this treatise is to provide a platform in which primary providers can
- Recognize the differences between congenital ear malformations and deformations
- Recognize the clinical subtypes of deformations
- Understand the physiology of the neonatal ear and the changes it undergoes in the first weeks of life
- Be cognizant of the types of external ear mold- ing systems available and their applications, limitations, and shortcomings
- Be able to treat ear deformities early in life with- out the need for a specialist consultation with the goal of obviating the need for costly, inconve- nient, and often painful surgical procedures later in life
- Often correct the deformity to a degree that it is superior to those that can be achieved by surgical treatment
Normal Ear Anatomy
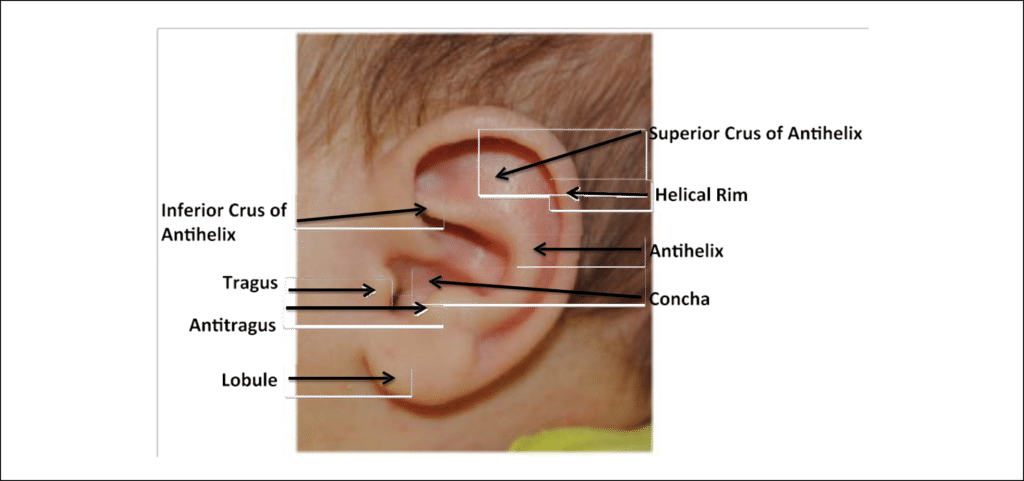
For the purposes of discussion of treatment options and in dealing with parents and patients who may have researched their child’s ear condition, it is important that pediatricians have a rudimentary knowledge of external ear (pinna, auricle) anatomy (Figure 1).
Contribution of the Pinna to Hearing and Appearance
The auricle or pinna, consists of a framework of cartilage and skin that is distinct from individual to individual.1 The appearance of the pinna is important for the aes- thetic balance of the face. In addition to the aesthetic appearance of the ear, children with ear deformations can go on to develop serious emotional and psycho- logical problems.2,3 It has been observed that children and adults with ear deformities experience signifi- cantly more anxiety, behavioral issues, psychological distress, and social avoidance than those with normal ear architecture.2,4-9 With early diagnosis and early treatment, surgical intervention can be avoided as well as undue psychological and social angst for the child.
1Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA
2Children’s Hospital of Philadelphia, PA, USA
Corresponding Author:
Catherine S. Chang, Division of Plastic and Reconstructive Surgery, Massachusetts General Hospital, Harvard Medical School, 55 Fruit Street, Wang 4-435, Boston, MA 02114, USA.
Email: catchangmd@gmail.com
In addition to contributing to a normal appearance, the pinna is functionally important in spatial hearing, or the ability to localize sound in space.1 A normal pinna architecture allows for reflection, shadowing, dispersion, diffraction, interference, and resonance, called pinna ques. These pinna ques are important for safety (ie, locating a sound direction in traffic) and accuracy when listening in a crowd. “Localization gives listeners the ability to construct auditory scenes of their surroundings, which reinforce their sense of space and their relationship with auditory objects in their surroundings.”10
Malformation Versus Deformation
Congenital ear anomalies are typically broken down into 2 main categories: malformations and deforma- tions. Ear malformations are conditions in which there is a deficiency in one or more auricular components (cartilage, skin, or soft tissue) due to abnormal embryo- logic development between the fifth and ninth weeks of gestation, thus resulting in an underdeveloped pinna.11- 13 When this is extreme the condition is often referred to as microtia or when all elements are missing, anotia. In contrast, ear deformations are conditions in which all (or mostly all) ear components are present but they are just misshapen, folded, or pleated. Deformational anomalies may occur secondary to in utero or ex utero external forces such as pressure from the birth canal or malposition when sleeping.13
The incidence of ear deformation in newborns has been documented in several studies and varies between 6% and 58%.3,12,14,15 Earlier studies reported an inci- dence around 20% when taken in aggregate, while later studies report an incidence as high as 58%.4,12,15,16 It appears that either this incidence is increasing or observ- ers are being more diligent in their assessment, or a combination of the two.
In general, ear deformations can be placed in 5 major subcategories:
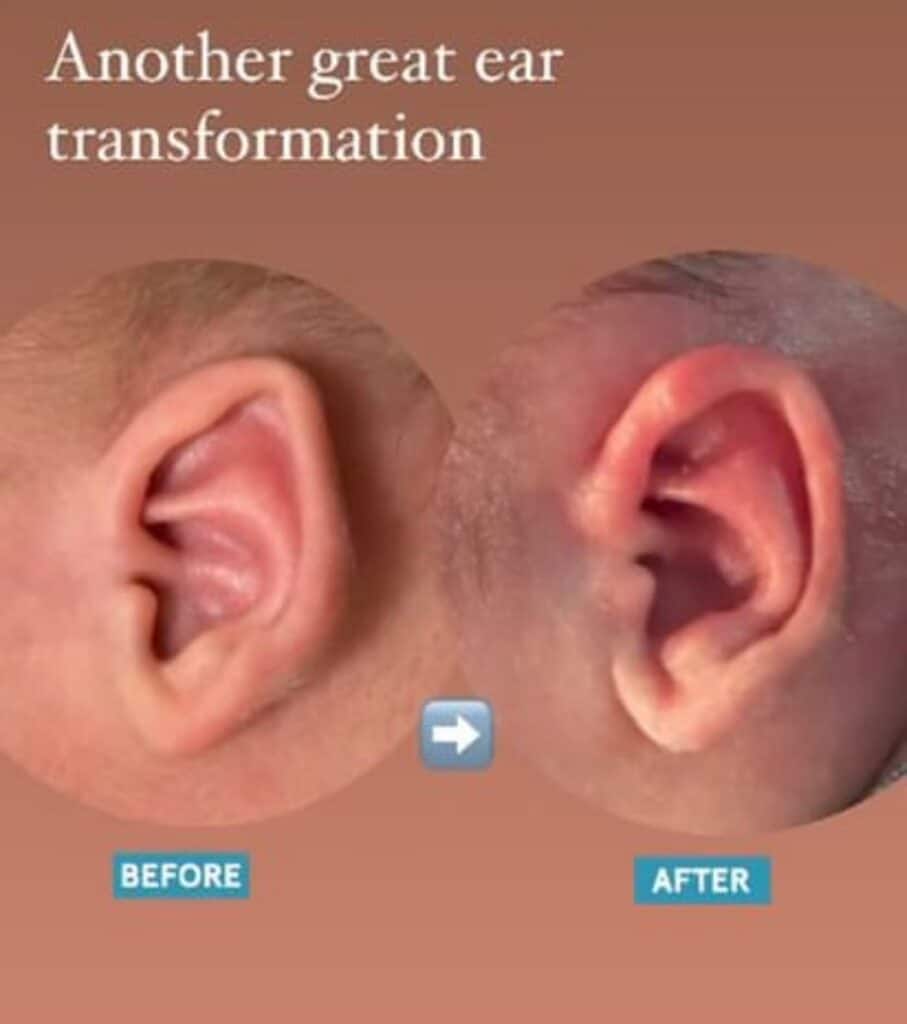
- Prominent ears: Ears that stick out or project well beyond the normal plane of the ear. This is usually due to enlargement of the conchal carti- lage or effacement of the antihelical fold or both (Figure 2).
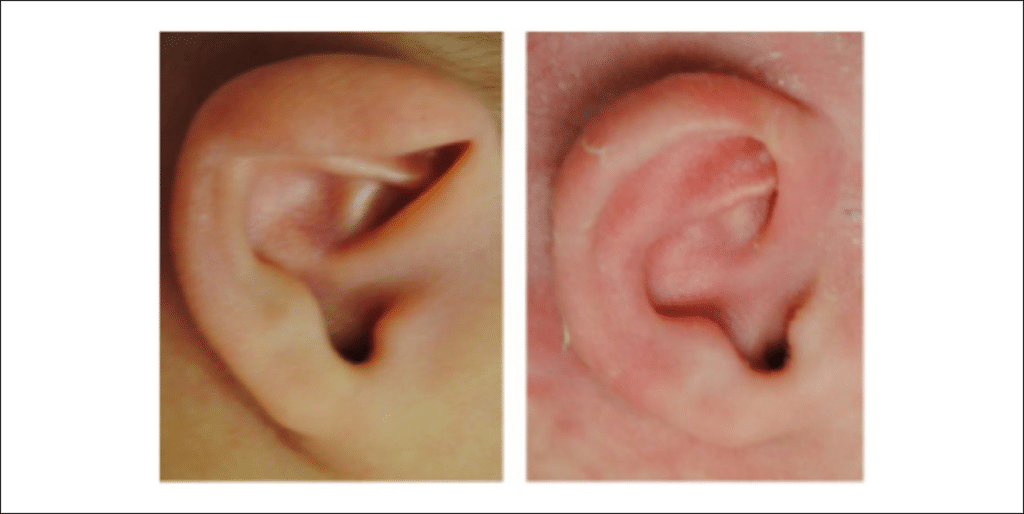
- Stahl’s deformity: Characterized by a third crus of the antihelix, which courses to the helical rim above the superior and inferior crus and causes effacement of the helical rim (Figure 3).
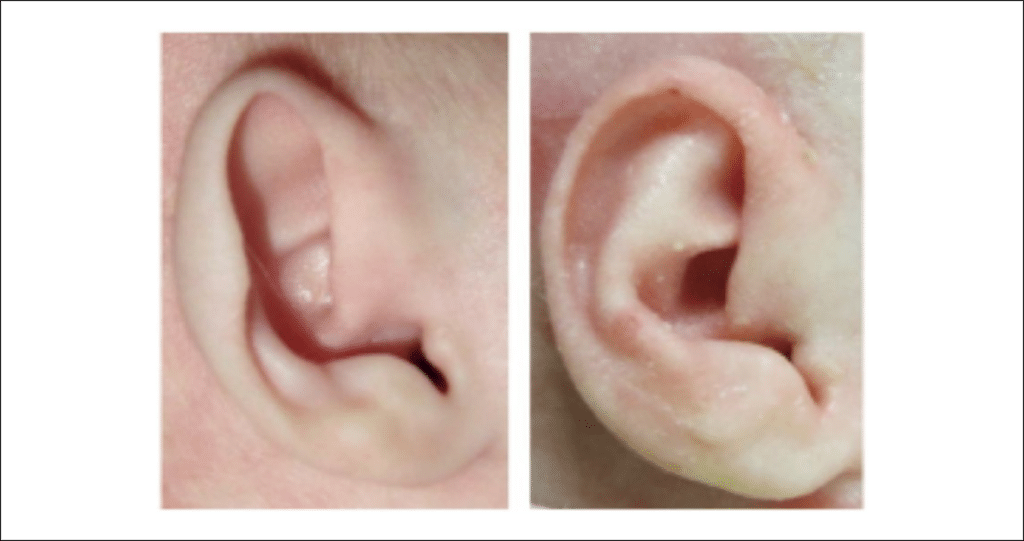
- Cup or lop ears are seen when the superior por- tion of the helix is folded down and over the anti- helix (Figure 4).
- Cryptotia is a condition in which the upper por- tion of the helix is buried under the temporal skin. By gently pulling the ear posteriorly a nor- mal ear form is seen (Figure 5).
- Helical rim anomalies are those in which the helix is folded or pleated or has an irregular curve (Figure 6).

Not infrequently, 2 or more types may be combined in a single patient representing a complex, mixed, or combi- nation deformity.
Of special consideration are a group of anomalies, which go by the heading of constricted ears (Figure 7). Strictly speaking, these ears are malformations in that there is a cartilaginous and soft tissue deficiency. The ear appears as if it has been crimped inward by a purse- string-type effect and they are typically smaller than normal. In addition to this deficiency they may be folded or pleated. The importance of recognizing this subgroup is that although they are mixed malformations and deformations, the deformational component may be improved with molding (see below).

Neonatal Ear Physiology
Maternal estrogen levels peak at or near delivery and these hormones cross the placental barrier resulting in high estrogen levels in the fetus as well. High estrogen levels cause increased cartilage pliability in the pubic symphysis of the mother and in the ears and noses of fetuses. Cartilage is a matrix composed of cells (chon- drocytes) and an intercellular matrix made up of colla- gen, proteoglycans, and some elastins. Estrogens work indirectly by increasing hyaluronic acid levels, which decreases cartilage elasticity and, hence, makes it less elastic and more pliable or conformable.15,17-19 This facil- itates delivery of the fetus by softening facial cartilage of the ear and nose. It is during this early post birth stage that deformed cartilages can be molded into a more nor- mal shape by the application of an external force in the form of an ear molding device. After 3 days maternal estrogen begins to decline and decrease to levels seen in older children by 6 weeks resulting in cartilage that is more firm and less elastic, thereby closing the window on the ability to mold the ear nonsurgically.12,20 Breastfeeding tends to extend the window to mold, most likely from the presence of maternal estrogen in breast milk.12


The Natural History of Untreated Ear Deformities
If left untreated, a percentage of these ear deformities may spontaneously self-correct (30%)12; however, it is currently impossible to predict which will do so. In 1990, Matsuo et al followed 1000 Japanese babies from birth to 1 year of age. He observed that lop ear deformi- ties were the most common type of deformational ear anomaly occurring in 38.1% of newborns and found that approximately 84% will resolve spontaneously if left untreated. Stahl’s ear was the second most common ear deformity occurring in 8.7% of all newborns. Eighty- five percent of these deformities spontaneously resolved with the frequency changing to 1.3% by 1 year of age. He found that the prevalence of prominent ears to be 0.4% of newborns. If not corrected, the frequency has been shown to increase to 4.4% by 1 month of age and 5.5% by 1 year of age. The of prevalence of cryptotia was found to be 0.2% and did not spontaneously correct.21
In 2017, Zhao et al reported a prospective study of 1500 newborns and carefully examined their ears at 7 days and 30 days of life.16 The incidence of all deforma- tional anomalies was 57.46% with spontaneous correc- tion of 31.55% of this cohort at 1 month, leaving 39.33% uncorrected. Gender, maternal age, and history of paren- tal smoking/alcohol use were not found to be significant risk factors for development of deformational ear defor- mities. However, 7 factors were found to be statistically significant: mother’s delivery situation (natural delivery vs cesarean), history of maternal hepatitis history, abnor- mal pregnancy (oligohydramnios, torsio funiculi umbi- lici, placenta previa), and neonatal weight greater than 4000 g. Cesarean delivery, newborn weight less than 2500 g, and a mother with no abnormal pregnancy or history of hepatitis were protective factors against devel- opment of an auricular deformity.16 This information can be very useful to help counsel parents prenatally.
Despite Matsuo and Zhang’s observation that some deformities self-correct, the majority it appears do not. For those patients, the only alternative is surgery, which is performed at age 5 years or older. Such surgery typi- cally involves a 1- to 3-hour operation, the wearing of a protective head wrap for 5 to 7 days postoperatively, the avoidance of sports for approximately 6 weeks, incom- plete correction, and of course the risk of bleeding, infection, and scars. As such, it is recommended that the diagnosis of an auricular deformational anomaly versus malformational anomaly be made at the time of birth and the neonate followed closely. If the deformity does not demonstrate correction by 1 week of life, ear mold- ing should be advised.4,12,15,22 If ear molding is initiated within 1 week of life, this can result in excellent correc- tion and avoidance of future surgery and can often lead to a more superior and natural result than surgery can accomplish.12,15,22
Ear Molding
Ear molding is a noninvasive, painless method of direct pressure applied to the deformational ear that serves to normalize the shape of the ear within a few weeks to months. The earlier the device is placed, the better the result and the shorter the duration of treatment, due to the cartilage pliability factors mentioned previously.4,12,15,22-27 Ear molding was first described in the 1980s by Matsuo and Korozumi using self-adhering Reston foam and Aluwax (a dental compound) and steri-strips. Other techniques of ear molding include using soft elastic dou- ble face loop padding, foam strips, thermoplast splints, wax mold and tape, silastic tubing with a wire core seg- ment, and adherent skin strips.2,3,5,11,15,19,25,26 In 1990, the Ear Well system was developed, which involved using a hard plastic stent, conformer, and plastic cap.12 The dif- ficulty with all of these techniques and devices is that they require early diagnosis and a separate visit to an ear specialist that can apply the device. InfantEar was intro- duced in 2017 and was designed for the pediatrician or nurse practitioner without having to defer to an ear spe- cialist allowing for earlier initiation of treatment.22
Commercially Available Products
Commercially available devices include Ear Buddies, Otostick, Ear Well, and InfantEar. Ear Buddies are mar- keted directly to parents, and include a flexible rim wire and tape to be applied by the parents. Although simple in its design, its application is tedious and it does not treat the full range of deformities observed. Additionally, put- ting the treatment in the hands of parents who are not familiar with ear deformities may be problematic.
Otostick is a simple 2-sided tape designed only for ear prominence only in children beyond the age of 3 months and to be applied by parents. This device is likely efficacious but has not been shown to be so in peer-reviewed studies. Waiting until 3 months of age will be less effective than in newborns with ear promi- nence. However, as it has been shown that the incidence of ear prominence increases during the first year of life, this device may have a role to play.15
Ear Well is a system designed for specialists (otolar- yngologists, plastic surgeons) and consists of a fixed outer framework and conformers to mold and shape the ear, and a cap. Although efficacious it comes in only 2 sizes that may not fit the infant’s ears, and requires a complicated series of steps for maximum benefit.
InfantEar differs from the Ear Well in that its design avoids direct pressure on the ear. It is designed for pedi- atricians and uses a series of progressive steps to reshape the ear beginning with a base piece, and adding con- formers, a new stabilization piece, and is contoured to each ear with the addition of a soft silicone gel that holds all the components together on curing. It is easy to apply and gives excellent results in the majority of patients. Similarly to other ear molding devices, it can cause minor skin irritation when wet or soiled.
Importance of Early Initiation of Ear Molding
Although ear molding has been in use since the early 1980s, its widespread acceptance has been hampered by delays in proper diagnosis, the accessibility of suitable molding materials, and the incorrect assumption that these deformities will self-correct.4,7,12,15,28 Despite numerous studies demonstrating efficacy of ear molding few parents have traditionally elected early nonsurgical treatment, most often due to a lack of information.16
Early correction is instrumental to a good out- come.4,12,22,23 Doft et al demonstrated that 96% of ear deformities were corrected and that treatment time can be reduced from 6 to 8 weeks to 2 weeks if molding is initi- ated within the first 2 weeks of life. In addition, with delay in treatment, treatment times are increased (3 to 12 months) with worse correction rates ranging from 18% to 70%.4
Despite their bulky and seemingly cumbersome appearance, ear molding devices are extremely safe, simple, and unimposing on the daily activities for the infant and the parents. When the caregivers of 100 infants who received ear molding were surveyed, 100% of participants rated the procedure as simple, 70% rated the result as “excellent,” 0% did not note increased irri- tability of the infant, and 99% of parents reported that they would repeat molding. The majority also noted that breastfeeding was not hindered with molding and that the device did not cause negative public attention.4 When given the option of 30% chance of spontaneous correction versus a 90% chance of improvement of the deformity with an ear molding procedure, parents were quick to choose the low-risk intervention.4
The benefits of early nonsurgical intervention of congenital ear deformities cannot be disputed. Besides the obvious avoidance of surgery, the procedure is low risk, painless, and has a decreased rate of residual deformity of the ear when compared with surgery (4% vs 10% to 24% with surgery).4 At this time, given that clinicians are unable to predict which ear deformities will self-correct, we recommend treating all deformi- ties with ear molding within the first week of life as there is little downside and a significant upside.4,12
Conclusion
Recognizing the different types of congenital ear deformities is paramount as it influences patient man- agement (surgical vs nonsurgical) and ultimately long- term patient and parental satisfaction. Deformational ear anomalies can be successfully treated nonsurgi- cally if such therapy is initiated within the first weeks of life. All clinicians evaluating neonates should be aware of the different types of ear deformities and the importance of early nonsurgical intervention.
Author Contributions
CSC and SPB both conceptualized and designed the paper, carried out the data collection, reviewed and revised the manuscript, and approved the final manuscript as submitted. Both authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publi- cation of this article: Dr. Bartlett is the founder and partial owner of TalexMedical, LLC, maker of InfantEar. Dr. Chang has no disclosures.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Catherine S. Chang https://orcid.org/0000-0002-6829-6421
References
- Blauert J. Spatial Hearing: The Psychophysics of Human Sound Localization. Cambridge, MA: MIT Press; 1983.
- Merlob P, Eshel Y, Mor N. Splinting therapy for congeni- tal auricular deformities with the use of soft material. J Perinatol. 1995;15:293-296.
- Smith W, Toye J, Reid A, Smith R. Nonsurgical correc- tion of congenital ear abnormalities in the newborn: case series. Paediatr Child Health. 2005;10:327-331.
- Doft MA, Goodkind AB, Diamond S, DiPace JI, Kacker A, LaBruna AN. The newborn butterfly project: a short- ened treatment protocol for ear molding. Plast Reconstr Surg. 2015;135:577e-583e.
- Kurozumi N, Ono S, Ishida H. Non-surgical correction of a congenital lop ear deformity by splinting with Reston foam. Br J Plast Surg. 1982;35:181-182.
- Bradbury ET, Hewison J, Timmons MJ. Psychological and social outcome of prominent ear correction in chil- dren. Br J Plast Surg. 1992;45:97-100.
- Furnas DW. Nonsurgical treatment of auricular defor- mities in neonates and infants. Pediatr Ann. 1999;28: 387-390.
- Spinelli HM. Congenital ear deformities. Pediatr Rev. 1993;14:473-474.
- Tan ST, Shibu M, Gault DT. A splint for correction of congenital ear deformities. Br J Plast Surg. 1994;47: 575-578.
- Stern RM, Brown GJ, Wang D. Binaural sound localiza- tion. In: Wang D, Brown DJ, eds. Computational Auditory Scene Analysis: Principles, Algorithms and Applications. Hoboken, NJ: John Wiley; 2006:147-186.
- Lindford AJ, Hettiaratchy S, Schonauer F. Postpartum splinting of ear deformities. BMJ. 2007;334:366-368.
- Byrd HS, Langevin CJ, Ghidoni LA. Ear molding in new- born infants with auricular deformities. Plast Reconstr Surg. 2010;126:1191-1200.
- Porter CJ, Tan ST. Congenital auricular anomalies: topo- graphic anatomy, embryology, classification, and treat- ment strategies. Plast Reconstr Surg. 2005;115:1701-1712.
- Baker SBK, Anand R. Nonsurgical ear molding improves many anomalies with few complications. AAP News. https://www.aappublications.org/news/2016/12/06/ Ear120616.PublishedDecember6,2016.RetrievedApril5, 2019.
- Matsuo K, Hirose T, Tomono T, et al. Nonsurgical cor- rection of congenital auricular deformities in the early neonate: a preliminary report. Plastic Reconstr Surg. 1984;73:38-51.
- Zhao H, Ma L, Qi X, et al. A morphometric study of the newborn ear and an analysis of factors related to congenital auricular deformities. Plast Reconstr Surg. 2017;140:147-155.
- Sommarin Y, Heinegard D. Specific interaction between cartilage proteoglycans and hyaluronic acid at the chon- drocyte cell surface. Biochem J. 1983;214:777-784.
- Hascall VC, Heinegard D. Aggregation of cartilage proteoglycans. II. Oligosaccharide competitors of the proteoglycan-hyaluronic acid interaction. J Biol Chem. 1974;249:4242-4249.
- Brown AM. Congenital bilateral ear atresia; correction with plastic surgery and prostheses. Plast Reconstr Surg (1946). 1951;7:327-332.
- Tapan M, Bulam H, Igde M, Singin S, Unlu RE. A simple method of neonatal ear molding for treatment of Stahl ear deformity. J Craniofac Surg. 2015;26:e802-e803.
- Matsuo K, Hayashi R, Kiyono M, Hirose T, Netsu Y. Nonsurgical correction of congenital auricular deformi- ties. Clin Plast Surg. 1990;17:383-395.
- Chang CS, Bartlett SP. A simplified nonsurgical method for the correction of neonatal deformational auricular anomalies. Clin Pediatr (Phila). 2017;56:132-139.
- Tan S, Wright A, Hemphill A, Ashton K, Evans J. Correction of deformational auricular anomalies by moulding—results of a fast-track service. N Z Med J. 2003;116:U584.
- Zambudio G, Guirao MJ, Sanchez JM, Giron O, Ruiz JI, Gutierrez MA. Nonsurgical correction of congenital auricular deformities a new method of neonatal mold- ing and splinting [in Spanish]. Cir Pediatr. 2007;20: 139-142.
- Yotsuyanagi T, Yokoi K, Urushidate S, Sawada Y. Nonsurgical correction of congenital auricular deformities in children older than early neonates. Plast Reconstr Surg. 1998;101:907-914.
- Ullmann Y, Blazer S, Ramon Y, Blumenfeld I, Peled IJ. Early nonsurgical correction of congenital auricular deformities. Plast Reconstr Surg. 2002;109:907-915.
- Hall A, Ahmed T, Mehta D, Daya H. Customised ear moulds: a viable alternative to cosmetic ear surgery. Arch Dis Child. 2012;97:335.
- van Wijk MP, Breugem CC, Kon M. Non-surgical correc- tion of congenital deformities of the auricle: a systematic review of the literature. J Plast Reconstr Aesthet Surg. 2009;62:727-736.